Long sensory pathways
- September 15, 2025
- 2:03 pm
Summary
This lecture reviews long sensory pathways. Somatic sensations include vibration, proprioception, fine/crude touch, pain, and temperature. The dorsal column medial lemniscus (DCML) pathway carries vibration/proprioception via ipsilateral ascent; the anterolateral system (ALS/spinothalamic tract) carries pain/temperature contralaterally. Both use 3-neuron pathways. Sensory dissociation occurs with selective tract lesions. Clinical anatomy examples highlight lesion effects.
Raw Transcript
[00:00] Okay, let's talk about long sensory pathways and answer the questions. What are the different types of somatic sensation? What tracks convey somatic sensations to the brain? And what are the ALS and DCML systems? Hello everyone. My name is Dr. Morton and I'm the noted anatomist. So first of all, sensation is the awareness of a stimulus.
[00:20] as a result of its perception by sensory receptors which then send that message to the brain, specifically the post-central gyrus of the primary sensory cortex of the parietal lobe. So a receptor is stimulated, that sensation is relayed by neurons to the spinal cord, then
[00:40] to the thalamus, then to the cerebral cortex where a shing consciousness is perceived. Let's do it another way. If the X in this picture represents a nerve lesion, then identify the symptom or symptoms this patient would most likely present with. Well, that is the dorsal root ganglion.
[01:00] ganglion, which means that's a dorsal root. They only contain sensory neurons. So if you knock out the dorsal root, you knock out all sensory neurons and therefore sensation is lost from that side of the body from that segmental level. Now, what do we mean by sensation? Somatic sensation now can be divided into
[01:20] the following different sensations clinically. Vibratory sensation, proprioception, fine, discriminative touch, pain, temperature, and crude, non-discriminative touch. So first, what is a receptor? Well, it's a transducer. Now that term, you probably know it, you just don't
[01:40] No, it is things like solar panels on your house that converts light energy from the sun into electrical energy or a windmill which converts wind energy that turns a combine and converts it into electrical energy. So a transducer converts a non-electrical stimulus into electricity. So things like light and vibration, so if you have
[02:00] photoenergy that hits your retina and that's turned into a neuronal action potential or a vibration that hits a part of your tendon and then that's turned into an action potential. So there are five different types of receptors in the body, mechanoreceptors that measure movement, nociceptors which are for pain.
[02:20] thermoreceptors that measure for temperature, chemo receptors that take chemicals and convert it to an action potential, and photoreceptors that convert light energy into an action potential. Now when it comes to long sensory pathways we just focus on these top three. Some receptors are specific to single modality.
[02:40] and some are a combination. So an example, esterognosis is when you reach into your pocket and you feel your keys, you can't see them but you feel it's cold, you feel the sharp and rough and smooth edges and you can recognize it's hard or soft. So there's more than one sensation that lets you know.
[03:00] what it is. Now sensation, here we've got each sensation is transmitted by sensory neurons, these sensory neurons through the dorsal root. Now what part of the spinal cord is utilized for these sensory pathways to reach the cerebral cortex? And the answer is spinal cord white matter.
[03:20] ascending tracts that go up. So in a nutshell, spinal cord white matter transports somatic sensory input up to the cerebral cortex. Now why do we care about the different types of sensation? Well the spinal cord white matter contains two major
[03:40] ascending pathways for somatic sensation. One is called the dorsal column media ligniscus and the other is called the anti-lateral system. So when we see the dorsal column media ligniscus, there it is, it's in the dorsal column of the spinal cord and it's transporting vibration.
[04:00] proprioception, and fine touch up the dorsal column. And so we see that all those sensory neurons go through the dorsal root, but then they ascend in the ipsilateral, same side, spinal cord, white matter. In contrast, the anterior lateral system gets its name because it's going up the
[04:20] and your lateral parts of the spinal cord white matter. And it specifically deals with pain temperature and crude touch. So those sensory neurons, all are going to then enter also through the dorsal root, but they're going to ascend in the contralateral spinal cord white matter.
[04:40] So, vibration and proprioception, and pain and temperature. Hey, why didn't you include fine touch and crude touch? Well, touch is subjective. Patients may not know how to explain the difference between them. So not that they're not important clinically, but I'm going to focus on vibration, proprioception, pain, and temperature.
[05:00] So let's blow this up. So there's the dorsal column. That's vibration proprioception ascending from the same side. And there's the anti-lateral system for pain and temperature from the opposite side. This is what's called sensory dissociation, where pain and temperature pathways ascend in the spinal cord separately.
[05:20] vibration and proprioception. Now how many neurons do the DCML and ALS systems use to get from the skin to the cerebral cortex like that? This is a three neuron pathway, a first, second, and third order neuron. Sensation goes in a first order neuron.
[05:40] second-order neuron, and a third-order neuron. The first-order neuron cell body is in the dorsal root ganglion, the cell body for the second-order neuron is in the spinal cord or spinal medullary junction, and then the cell body for the third-order neuron is in the thalamus. There's a decissation that a
[06:00] occurs somewhere in all second order neurons. Now that term decasate is where axons cross from one side of the brain or spinal cord to the other. And this word decasate is Latin for mark with a cross because the Roman numeral X is deca as in X which
[06:20] shows crossing from one side to the other. Now let's go over the anti-lateral system and dorsal column medial luniscus individually. So let's first start with the ALS, shall we? Also known as the spinal thalamic tract. This is going to be for pain and temperature pathway and there's three neurons, first order, second order, and third order neuron.
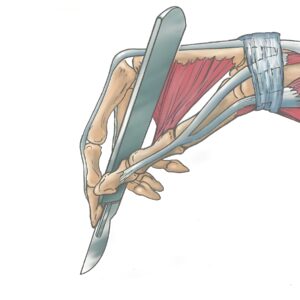
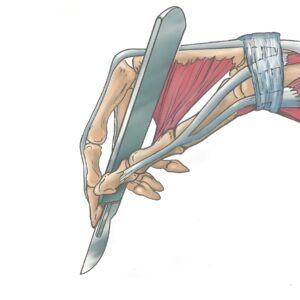
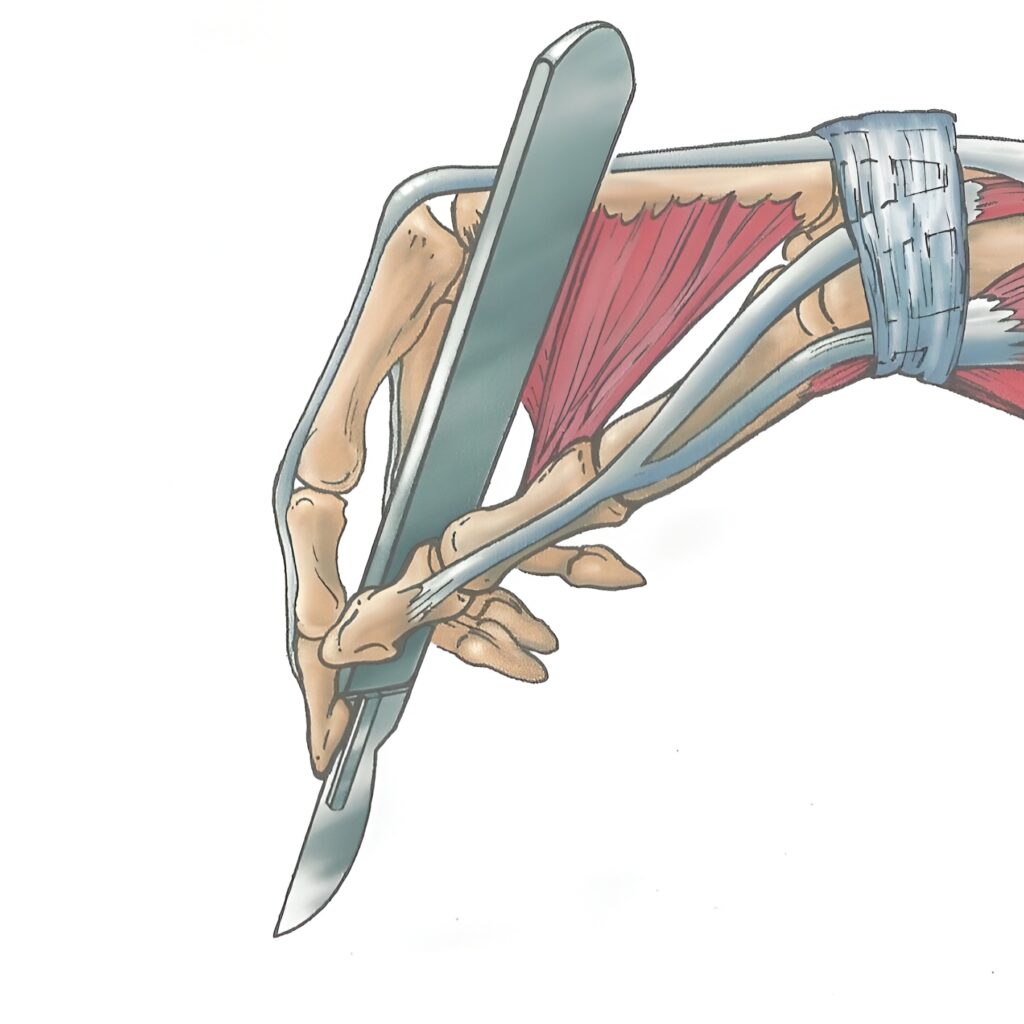
[06:40] But I'm going to draw them this way, okay, where the first-order neuron is coming from somewhere in the skin. In this case, I'm doing it the skin over the medial malleolus and then I'm going to take this pin and poke the skin. And that primary-order neuron is going to enter through the dorsal root and go into the dorsal horn, or that central horn.
[07:00] second-order neuron decisates in something called the anterior white commissure to the contralateral side of the spinal cord and to send in the anterior lateral system to synapse in the thalamus where third-order neuron will course into the cerebral cortex. Now why is it called the anterior lateral
[07:20] system? Well, there's the antior lateral system. It's located in the anterior lateral portion of spinal cord white matter. Why is it also called the spinal thalamic tract? Because part of the tract courses from the spinal cord to the thalamus. Now that was fun.
[07:40] Wasn't it? Let's do it again. So here we're going to show this illustration that I did where there's the cerebrum and there's the thalamus and then midbrain, pons, medulla, and then there's the cervical, thoracic, lumbar, and sacral spinal cord levels. Now what we're going to do is take a cross section through the lumbar and one through the thoracic and one through the cervical and
[08:00] We also end that spinal medullary junction and then a cross section through medulla pons, midbrain and then a coronal section through the cerebral cortex and thalamus and show right and left sides. That's the model we're going to use to relay the pain and temperature. So there's our three order neurons, but now we're going
[08:20] to do it again. Where there we have primary neuron in the dorsal root ganglion going to the dorsal horn like this. Ouch. Okay. And we're poking for pain. So there's a primary order neuron that choruses to the dorsal root ganglion where the cell body is, synapses in the dorsal horn.
[08:40] Then that second order neuron is going to decasate at the anterior white commissure, go through the spinal thalamic tract in synapse and the thalamus. So there is the second order neuron cell body in the dorsal horn gray matter. It decasates at the anterior white commissure and then ascends and the spinal
[09:00] the spinal thalamic tract all the way through the brainstem and then synapses in the thalamus. And from the thalamus, that third order neuron goes to the primary sensory cortex. Third order neuron courses through the internal capsule and then synapses in the postcentral gyrus of the cerebral cortex.
[09:20] So what we're going to do is I'm going to take a little bit of a tangent and talk about something called the sensory homunculus. It's a distorted brain map of sensory distribution of the human body and there you can see the foot and going up to the leg and the trunk all the way up to your upper limb and hand into the head, face, tongue.
[09:40] region. Larger parts of the homunculus show more complex innervation, so the amount of cortex devoted to body region is not proportional to its associated surface area. So for example, you see how big the hand is compared to how small the foot is? That's showing that there's a larger, there's more complex
[10:00] innervation in the hand than in the foot. So there we see that the sensation is on the medial malleolus and that's why the sensation is going to the medial part of the longitudinal cerebral fissure like is shown there. It's like a map. Alright, so
[10:20] There we have it shown in three-order neurons and there we have the three-order neurons demonstrated. Now there's something here I put up the tract of Lisauer that I'm not spending a lot of time on, but I'm going to spend some time. Okay, so here we have skin and there's pain and temperature for if primary order neuron comes in, synapses in the dorsal horn and.
[10:40] second order neuron decosates to the opposite side and it's going to continue up. But there's something called the tract of lissaur or dorsal lateral tract. And this is where central processes of first order neurons may branch within this lissaur's tract at the tip of the dorsal horn and then that central process can ascend or descend
[11:00] in the sours tract for two or three spinal cord segments to synapse with second-order neurons in the dorsal horn of a superior inferior adjacent spinal cord. So let's do that again. So there's a primary order neuron from L4 and when it enters, instead of synapsing some of these central processes ascend up to a superior segment and then
[11:20] synapse with a second-order neuron in a superior level of the spinal cord. But take a look at what also happens below, in this case the L5 level. That primary order neuron enters Lisauer's tract and then it ascends up two segments to synapse in the L3 segment with that second-order neuron.
[11:40] Now why should we care about this? Well if we have a lesion right there on the L4 spinal cord level on the anti-lateral system, the sensation from that level and perhaps the level below may remain intact.
[12:00] because Lisauer's tract allows that sensation to ascend up two or three segments. That makes sense? All right. Now let's do some practice time for ALS. Where would pain and temperature sensory loss occur if the left antilateral system and the L-force spinal cord region were damaged?
[12:20] We've got it right there. And so I'm going to go and answer this, but you may want to take a second to think this over. But if we see sensation from any level below that, it'll go up. It can't get up, cannot get up because there's a lesion in the anti-lateral system. But now let's go from the cervical region. Watch.
[12:40] what happens from the contralateral side, sensation has no problem coming in, either from the T4 level, but what happens at the L4 level is some of that material, that sensation will not make it and definitely from the sacral region will not make it like that. So pain and temperature from the contralateral
[13:00] side of the body at or below the lesion cannot make it to the brain and if the brain cannot perceive the sensation coming in that input then the brain does not recognize sensation occurred. So if the sensations in the left antilateral system then we'll have right-sided
[13:20] loss of pain and temperature at and below that level. Let's do another one. The indicated region has no pain sensation. Vibratory sensation is unaffected. Identify the part of the CNS most likely damaged. Well, I'm going to give you these choices and pause to answer, but I'm going to go ahead and answer.
[13:40] So sensation, loss of pain and temperature on the left side of the body. And so the lateral medulla conveys pain and temperature sensation from the contralateral side of the body. And so A would be the best answer. That is the best answer as shown here because skin for pain and temperature from the
[14:00] contralateral side of the body ascends up the anti-lateral system to the medulla like that. The cervical region from B and E are not correct because B does not, at the C7 level, does not include, based upon the dermatomes, affected enough segmental levels and E is on the wrong side. C is
[14:20] is showing not enough dermatomes on the right and left is the wrong side. All those are the wrong side. Take a breather, stand up, crack your knuckles, and let's go to the dorsal column medial meniscus, which is Vibration and Proprioception Pathway through Three Neurons, 1 to 2.
[14:40] 2 and 3. So we're going to show the same coming from the medial malleolus, the L4 spinal cord level. But instead of a pin for pain, we're going to do a tuning fork for vibration. And that primary order neuron also enters through the dorsal root. But then that dorsal column is where that neuron ascends.
[15:00] to send out to the second-order neuron in the spinal medullary junction and then to send up contralateral to the constralateral thalamus where third-order neuron will go to the cerebral cortex. Now why is it called the dorsal column medial ligniscus? Well that's the dorsal column of the spinal cord and the medial ligniscus
[15:20] is Greek for ribbon because in the brainstem the ascending neurons altogether spiral like a ribbon. It's quite pretty actually, like that. Now that was fun. Let's do it again except with more detail. Their skin and when vibration or pressure
[15:40] proprioception or stimulated, those primary order neurons enter through the dorsal root, there's the cell body for the dorsal root ganglion, they're going to ascend and synapse in the spinal medullary junction like this. So there we're going to vibratory sensation on the medial malleolus and a primary order neuron will enter through the dorsal
[16:00] root ganglion and then in the dorsal column ascend up that ipsilateral side, still the primary order neuron, in the gracile fasciculus. But there's also the cuneate fasciculus. And then that, I'm going to talk about those in a second, in that primary order neuron is going to synapse in the gracile
[16:20] nucleus, but there's also a cuneate nucleus. What's the deal with those? Well, let's take a second and blow that up and talk about it. The gracile fasciculus is a part of the dorsal column and gracile is Greek for slender like the gracilis muscle and the medial part of the thigh is very slender.
[16:40] Pesticulus means bundle. So this slender bundle is going to transport primary order neurons that are carrying vibration and proprioception from below the T7 spinal cord level up to the spinal medullary junction. Specifically the gracile nucleus where the synapse occurs. Gracile phesiculus
[17:00] synapses in the gracile nucleus. The gracile tract is identifiable on every section of the spinal cord. Now in contrast, the cuneate fasciculus, which is Latin for wedge and bundle of wedge-shaped axons, transport vibration and proprioception from
[17:20] above the T6 spinal cord level and then those primary order neurons synapse in the cuneate nucleus and the cuneate tract is identifiable only on the upper sections of the spinal cord above T6. So there's those two fascicles which together make the dorsal column.
[17:40] And the gracile nucleus and cuneate nucleus are the cell bodies for second-order neurons, the synapse between the first and second-order neuron. So there's that spinal medullary junction. So now that we have this cuneate nucleus, or gracile nucleus, that second-order neuron is going to then
[18:00] decasate at the spinal medullary junction and then ascend in the medial ligniscus to synapse in the thalamus. So there's that second order neuron. It's going to decasate at the spinal medullary junction and ascend in the contralateral medial ligniscus all through the brainstem and synapse
[18:20] in the contralateral thalamus. Then the third-order neuron is going to ascend to the primary sensory cortex. So there we have the cell body in the third-order neuron. It ascends up through the internal capsule in synapses in the postcentral gyrus. And there we have
[18:40] have all of them. I want to make a note here like a little caveat. Sematocensory information is oh hey Gabriel. Sorry my son Gabe just brought me very tasty sorbet. It's like I think it's mint no shirt it's lime it's very tasty.
[19:00] Thought I'd share that with you. Now the little caveat here is somatosensory information involved with proprioception and posture is also processed in the cerebellum. And we have these spinocerebellar tracks that are going to come and it helps to ensure that where our limbs are in location are actually perceived where they are at.
[19:20] but I'm going to leave that for another video. Alright, so there's the dorsal column, medium lineuscus, all three-order neurons. So let's do a little practice time, shall we? Where would vibratory sensory loss occur if the right DCML at the L4 spinal cord region were damaged? Okay, there. So pause the video
[19:40] video, but I'm going to go forward. So ascending information on the ipsilateral side is going to be problematic, but we see that ipsilateral information on rostral spinal cord segments are unaffected, but at the level and levels below are all going to be affected.
[20:00] So vibration and proprioception from the same side of the body at or below the lesion cannot get to the brain. And so if we're on the right DCML, we are going to then lose vibration and proprioception on the right side of the body from that level and down.
[20:20] Does that make sense? Let's do one more. The red shaded region of the spinal cord is injured. Identify the letter that most likely demonstrates loss of vibratory sensation in this patient. Well here we have a bunch of pictures. So pause, but I'm going to go forward. So the correct answer is D.
[20:40] Now, I know this is a thoracic spinal cord level because there's a lateral horn for preganglionic sympathetic neurons, a very small gray matter ventral horn because the intercostal and abdominal muscles do not require a lot of motor neurons, and there's quite a bit of white matter.
[21:00] So we know this is thoracic. Now A is wrong because it's showing dermatomes that are lost in the cervical region and this is a thoracic level. B is incorrect because it's showing only a dermatome probably from the C7 level that's injured and this is white matter. So far more dermatomes.
[21:20] affected. C is incorrect because it's also showing only one dermatome that is affected. And E is wrong that so even though it's a dermatome in the thoracic region, it's only one dermatome which is because the white matter is affected, there will be every dermatome below that would be injured.
[21:40] There we have it. Okay, injured spinal cord. Now what we're going to see in this case with a Hemicord or Brown-Sacord syndrome is the injury is on half the spinal cord. So they will lose, have loss of vibration and proprioception from the ipsilateral side of the body at and below the spinal cord lesion.
[22:00] However, they'll also have loss of pain and temperature from the contralateral side of the body at and below the spinal cord lesion. What do we call this phenomenon? Sensory dissociation. Remember, we talked about that before. Okay, let's do one more example. The indicated region has no vibratory sensation.
[22:20] shown here. Identify the part of the central nervous system most likely damaged and here are the choices. Pause but I'm going to go forward. So what we see here is the left side of the body and from cervical region all the way down has lost vibratory sensation on the left side of the body and because it's on the left side of the
[22:40] body and it's vibration that will be from the left side of the spinal cord and not brainstem because the brainstem is going to be from the opposite side. So it'll be the left side. So vibration from the same side of the body at or below the spinal cord region, G is the best answer here.
[23:00] As shown right there in red where you see the lesion on the left dorsal column showing that all sensation from the C4 spinal cord level down on the left side for vibration proprioception is lost. Okay, so here is a synopsis of the dorsal column medial ligniscus. Here is a synopsis of the dorsal column medial ligniscus.
[23:20] of the anti-lateral system and that my friends are the long sensory pathways in a nutshell.
[23:40] 🎵
[24:00] Thanks for watching.